The Allied Aeromedical Architecture
According to the NATO terminology database, Aeromedical Evacuation (AE) is the movement of patients under medical supervision by air transport to and between Medical Treatment Facilities (MTFs) as an integral part of the treatment continuum.1 In this definition, ‘patients’ refers to individuals admitted to care when entering the healthcare system for diagnosis or treatment, ‘medical supervision’ identifies the medical contribution in the regulating process of patients and ‘treatment continuum’ means the uninterrupted, progressive, and appropriate medical attention and response to the needs of patients throughout the chain of their medical treatment and evacuation. These three concepts together make AE a medical responsibility.
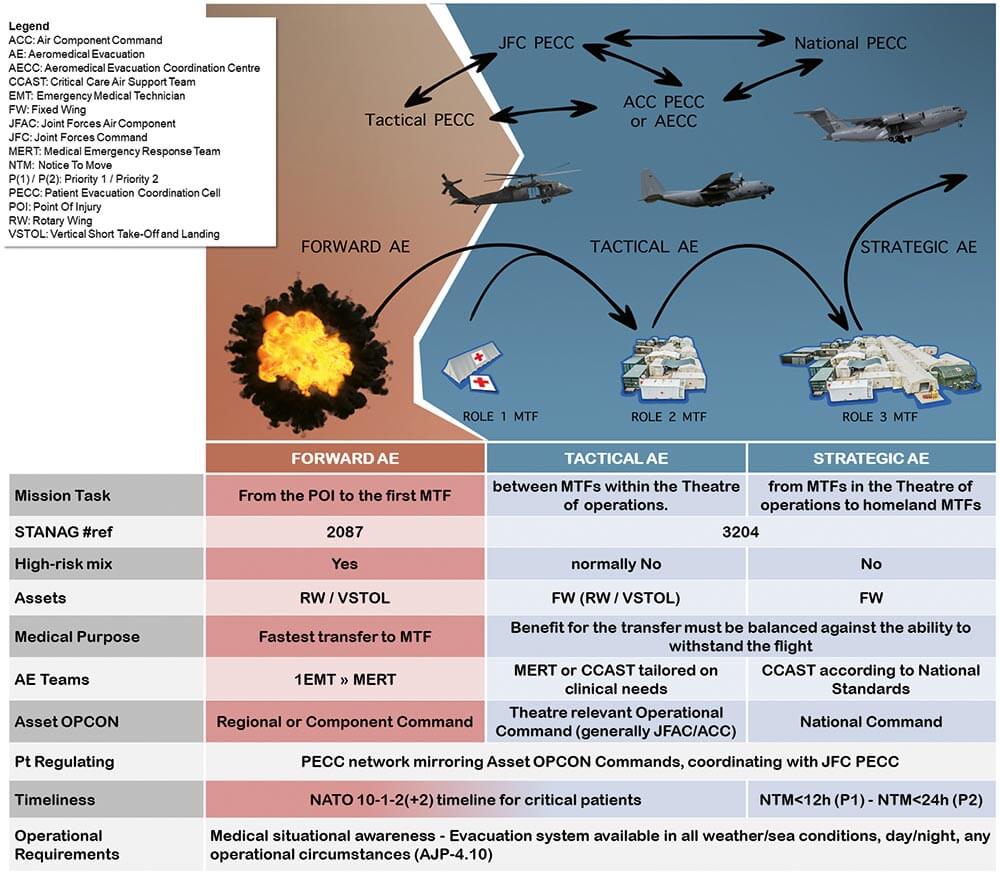
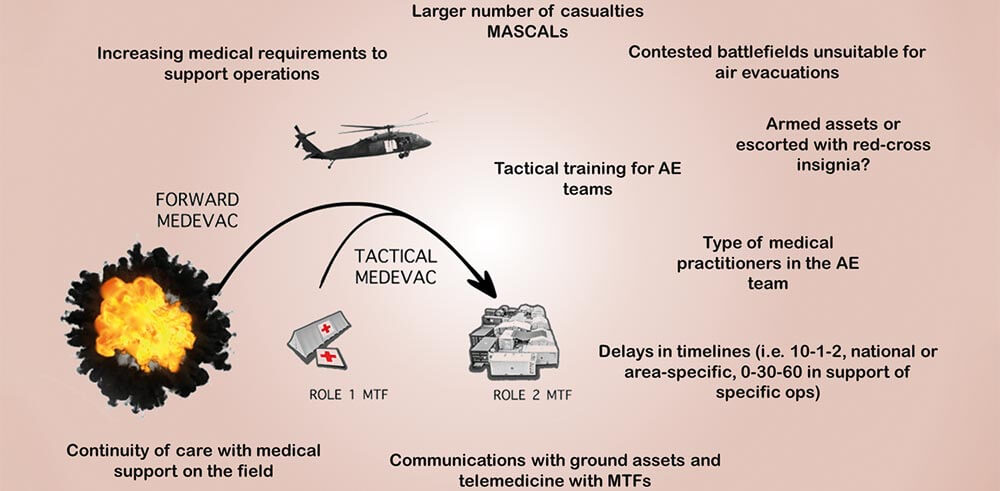
AE is divided in three phases.2
- Forward AE (FwdAE) provides ‘the movement of casualties in an air platform with medical personnel from point of injury and/or illness to the first medical treatment facility.’
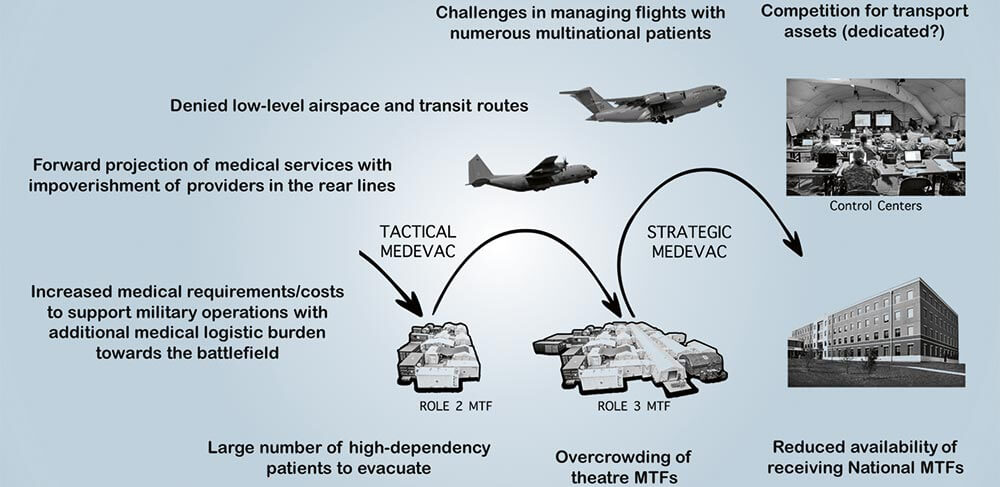
- Tactical AE (TacAE) represents ‘the intra-theatre movement of patients in an air platform with medical personnel between medical treatment facilities.’
- Strategic AE (StratAE) corresponds to ‘the inter-theatre movement of patients in an air platform under the supervision of medical personnel from the area of operations to medical treatment facilities outside the area of operations or between medical treatment facilities outside the area of operations.’
TacAE and StratAE are addressed by the same document, the Standardization Agreement (STANAG) 3204, due to their similarities in mission design.3 They are usually not high-risk missions, generally performed on FW assets after a formal fitness for flight travel is issued by a flight surgeon or a medical officer qualified in aerospace medicine. Patients are assessed against their condition to survive the air transfer and provided with the specific kind of en route care they need. AE Teams are selected to deliver in transit care in accordance with prevailing medical standards at the same or higher level as provided by the originating unit.4 Typically, Medical Emergency Response Teams (MERT) and Critical Care Air Support Teams (CCAST) are physician-led AE teams of doctors, nurses and technicians (mostly providers with a background in critical/intensive care, anaesthesiology and emergency medicine) trained by the Air Force to support high-dependency patients in-flight.5
Figure 1: The architecture of the AE system in the continuum of care and a possible flow of medical information in a deployed PECC network.
© LT Ákos Szénási
According to STANAG 2087, FwdAE is performed mainly by RW or VSTOL assets. The primary mission objective is the retrieval of severely injured casualties from the prehospital environment to a MTF as quickly as possible with essential on-board medical personnel.6 TacAE and StratAE missions are regulated respectively by Theatre, National and Multinational-level Operational Centres while FwdAE platforms are controlled by Regional or Component Commands.7 The proper medical information to determine the timeliness and the prioritization of transfers is provided by the network of Patient Evacuation Coordination Cells (PECC), which constantly monitors the readiness status of the healthcare facilities and assets, tracks patient movements and optimizes patient flows among different stages of care.8 Normally, each command establishes a PECC in the Joint Operations Centre (JOC) where the current medical situation is constantly updated for the competent commanding authority and JFC PECC. Air Commands generally include the PECC functions within the Aeromedical Evacuation Coordination Centre (AECC). The PECC reports to J3 for the execution of AE missions but has constant access to the Joint Medical (JMED) Branch for advice to ensure that the medical requirements are properly included in the planning, execution and adaptation phases of AE missions for each course of action.9
Allied Standards
AE systems have the advantage of connecting medical capabilities over a wide territory and facilitate the distribution of specialized resources. In order to comply with the agreed-upon allied standards, especially for the early stages of care in emergency situations, patients should access the proper MTF at the proper time. In modern allied warfare, air assets operate relative safety in the context of air supremacy, quickly connecting MTFs to the fighting force. The perception of a controllable operational risk encouraged the adoption of civilian prehospital standards (i.e. the golden hour principle) to improve patient outcomes as reasonable solutions, even for deployed military settings. One of the most successful improvements derived from the civilian legacy is the NATO 10-1-2(+2) timeline.10
The NATO 10-1-2(+2) timeline displays the critical interventions that need to be considered for completing all resuscitative stages in the continuum of care:
10 minutes of injury or onset of severe symptoms for bystanders to deliver effective first aid, bleeding and airway control to the most severely injured casualties.
1 hour of injury or onset of acute symptoms to provide medical service personnel, qualified, trained and equipped for emergency care to start advanced resuscitation and pre-hospital emergency care
2 hours of injury or onset of acute symptoms to provide medical service personnel qualified, trained and equipped for surgical and resuscitative emergency care to complement prehospital emergency care by life limb and function preserving surgical and resuscitative procedures as soon as possible
+2 hours of tactical evacuation after initial treatment to provide further surgical, resuscitative, diagnostic and specialist care capabilities necessary to stabilize the patient for strategic evacuation.
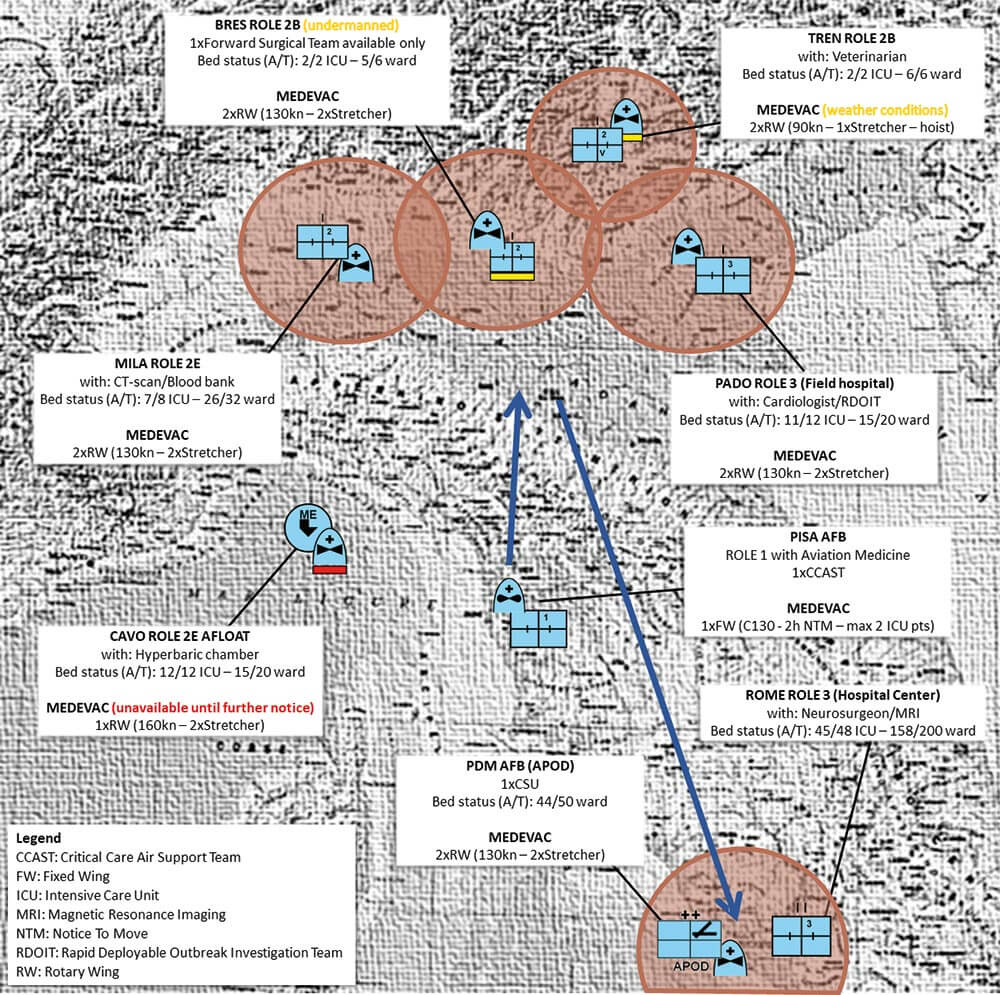
Those times are depicted on a map as Medical Evacuation (MEDEVAC) rings, representing the area of terrain that is covered by the AE platforms to deliver the agreed standard. MEDEVAC rings are the main determinants of the Medical Common Operational Picture (MEDCOP), a visual chart where medical infrastructure, core capabilities, readiness states and assets are displayed (Figure 2).
Figure 2: An example of MEDCOP (fictional), displaying medical assets and facilities with their most relevant features and updated readiness status.
© Dr Jacopo Frassini
It is important to note that the allied MEDEVAC rings are calculated from the moment of injury/sickness and represent the limit to provide initial surgery in a FwdAE loop. In order to show clinical information to medical decision makers, MEDEVAC rings not only represent the specifications of air assets (i.e. cruise speed), but also include other operational/medical variables, such as reporting times from the unit, processing of requests by the PECC/JOC, ground handling and care of patients until handover to the destination MTF. Different platforms offer different cabin arrangements, equipment, payload, total number of crew members and capacity to evacuate patients. Combinations of these options are important to enable a certain level of en route care and accomplish medical mission success.
The Nations perform StratAE according to the patient priority soon after the Patient Movement Request (PMR) is issued by the treating MTF or by the Casualty Staging Unit (CSU) for patients with minor conditions.11 When augmented with aerospace medicine capabilities, CSUs are commonly referred to as Aeromedical Staging Units (ASU), which are stationed at major air-hubs serving as buffers allowing stabilized patients to be rapidly prepared for flight as soon as aircraft become available. StratAE missions are long-range transfers of stabilized patients. The preparation of patients must be synchronized with the readiness of the assets and matched with the proper cabin configuration and on-board assistance. In these conditions, patient outcomes are related to the quality of the aeromedical support compared to speed of accessing the next level of intervention. StratAE is calculated in Notice to Move (NTM) times, identifying the limit to initiate the mission (i.e. less than 12 hours for a priority 1). Experience proved that patients can reach homeland facilities in less than 72 hours of wounding with an efficient coordination of the three stages of AE.
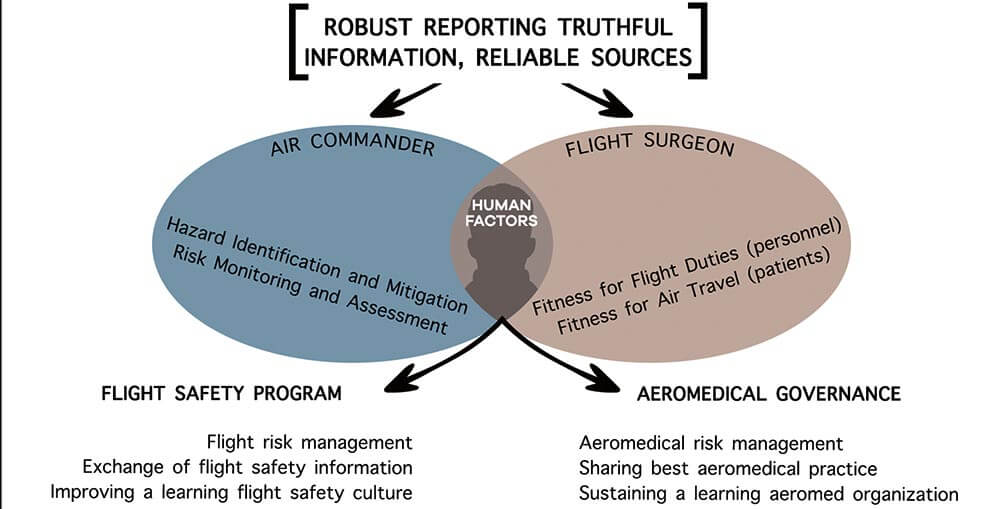
Figure 3: Similarities between a Flight Safety Program and an Aeromedical Governance Framework.
© LT Ákos Szénási
Shaping Quality in AE Systems
The three phases of AE are essential components in the modern design of a NATO healthcare architecture to the point that a standard allied evacuation system has been agreed to be available in all weather and sea conditions, at day and night, and in any operational circumstances.12 However, realistic limitations on readiness are very common due to safety concerns and reaction times become significantly longer than expected. Evacuation systems are flexible networks where ground, maritime and air assets are constantly adapted to deliver the continuum of care to the supported force. Generally accepted timelines can be used as planning references in order to best allocate medical resources and shape the deployed emergency medical system in the battlespace, yet some specific situations require dynamic approaches or dedicated solutions to still meet those standards or further optimize medical outcomes. Air operations must be effective, sustainable and safe, where safety in combat is not riskless, but free of preventable hazards. Risk management is conducted through a trusted reporting system better known as the Flight Safety Program13 that represents the main learning component in the allied aviation safety strategy to support decision-making processes of commanders at all levels. The Flight Safety Program is based on a direct channel of communication from flying units to decision makers concerning safety issues that might have endangered the mission and can contribute to maintain risk awareness adherent to evolving combat conditions. Information needs to be shared and passed from originators to higher formations so that the overall picture can be analyzed for wider application and harmonized among all contributors to enable safety outcomes. Remedial actions or simple recommendations are generated to improve collective awareness of a hazard, identify solutions and avoid the repetition of adverse occurrences. Aeromedical governance is a similar process applied by flight surgeons to deliver quality in AEs, so that patient outcomes are constantly monitored and optimized by integrating medical and operational solutions to accomplish specific clinical requirements.14 AE is a core component in modern healthcare support to operations, yet it represents only a part of the continuum of care that needs to be harmonized when connecting consecutive stages of the treatment chain from the battlefield to homeland hospitals.
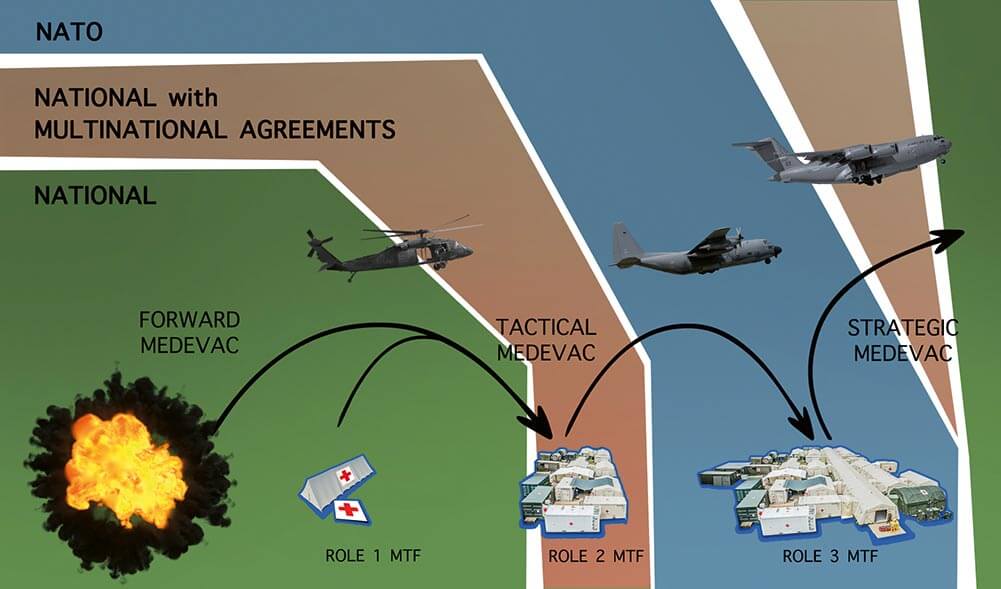
All medical inputs and outputs of operational commands cannot be fully effective without accountability in providing a continuous improvement of healthcare support. As outlined in Figure 4, the green area depicts the resulting main area of national responsibility for capability development and care delivery in NATO operations. The brown area shows where national accountability is shared among more Allied Nations operating in the same combat zone with pre-deployment agreements. In the blue area, the basic responsibility handed over to NATO commanders upon transfer of authority. Such a fragmented scenario poses a risk to aeromedical governance that should be able to fluently regulate casualties throughout the continuum of care. The provision of some kind of care alone does not directly imply best patient outcomes, most importantly in complex multinational environments.15
In Allied deployments, operational commanders face the difficult challenge to harmonize the medical common operational picture so that the resulting integrated system of care is enabled to guide and track patients over time through a comprehensive array of health services by consecutive and increasing levels of intensity of medical interventions.16 Performance indicators (i.e. MEDEVAC mission total time) are basic tools for assessing, monitoring and optimizing quality of care. In military systems, medicine is not a stand-alone discipline but needs strong integration in the command and control structure to provide medical support services that frequently result from a coordinated sequence of medical interventions delivered in different moments and places. As a consequence, performance indicators are a combination of clinical and operational figures and require unique expertise to correctly and effectively analyze their meaning in a combat environment.
Figure 4: A simplified separation of accountability in the provision of the continuum of care in allied operations.15
© LT Ákos Szénási
Outlook
Future challenges are strongly influenced by the evolution of warfare and combat threats. Hybrid warfare scenarios against increasing technologically capable adversaries in possibly denied areas of interventions will pose serious limitations to the flexibility of traditional aeromedical platforms to connect stages of care.17 In particular, constraints on availability and mobility of aeromedical assets will require a serious approach to alternative solutions to sustain the currently expected patient outcomes and the continuity of care. Some of the challenges may be prevalent in the FwdAE phase, which is the most exposed to low-level airspace threats. However, TactAE and StratAE phases will also encounter difficulties in the regular transfer of patients in contested battlespaces. In multinational environments, interoperability of assets, facilities, procedures, equipment and personnel is a key enabler of the healthcare support across the whole range of deployed capabilities.18 Recent studies showed how joining military forces with different backgrounds generates the risk of duplication, overcapacity and barriers in procurement that can reach 15 % of the total budget.19 All NATO countries together represent the world’s leading alliance in defence spending. However, multinational military systems like the EU use up to 17 different types of assets compared to single nation organizations like the US.20 Heterogeneity in the spectrum of available capabilities generates additional implied costs and increased organizational efforts for sustainment and interoperability during combined campaigns.
Figure 5: Illustrative list of possible AE challenges in the future global security environment.
© LT Ákos Szénási
Multinational healthcare systems require long-term planning of dedicated resources to support the operational requirements with the agreed standards of care. To achieve best patient outcomes, aeromedical capabilities need flexible development strategies to continuously harmonize technological progress, evolving evidence in medical practice and the context of future warfare scenarios. As advocated by the NATO Smart Defence initiative, multinational solutions must result from a coordinated planning approach, specialization/modularity and prioritization of investments across the Alliance.21 Consequently, Nations can synchronize individual projects cost-efficiently and grow cohesive understanding to meet the security challenges of the 21st century.
Conclusion
AE in NATO operations is a core enabling function for mission success. Its architecture as depicted in AJP-4.10 and related medical STANAGS ensures that a casualty is retrieved from the prehospital environment and transferred via the continuum of care through to rehabilitation. Allied aeromedical standards create the best agreed-upon conditions to deliver the right treatment in the right place at the right time. Best patient outcomes result when allied standards are continuously adapted to the battlespace and when the quality of healthcare can be monitored, analyzed and improved. However, AE assets cannot be improvized to accomplish their clinical support mission, especially in multinational contexts. Our recommendation is to consider AE as a dedicated medical support capability to be planned, developed, manned, trained, exercised and controlled collectively in order to achieve both economy of scale and optimized medical outcomes.
Acknowledgements
Special thanks to LT Ákos Szénási for the restyling of figures 1, 3, 4 and 5.